Under-Eye Hollowing & Tear Trough Deformity
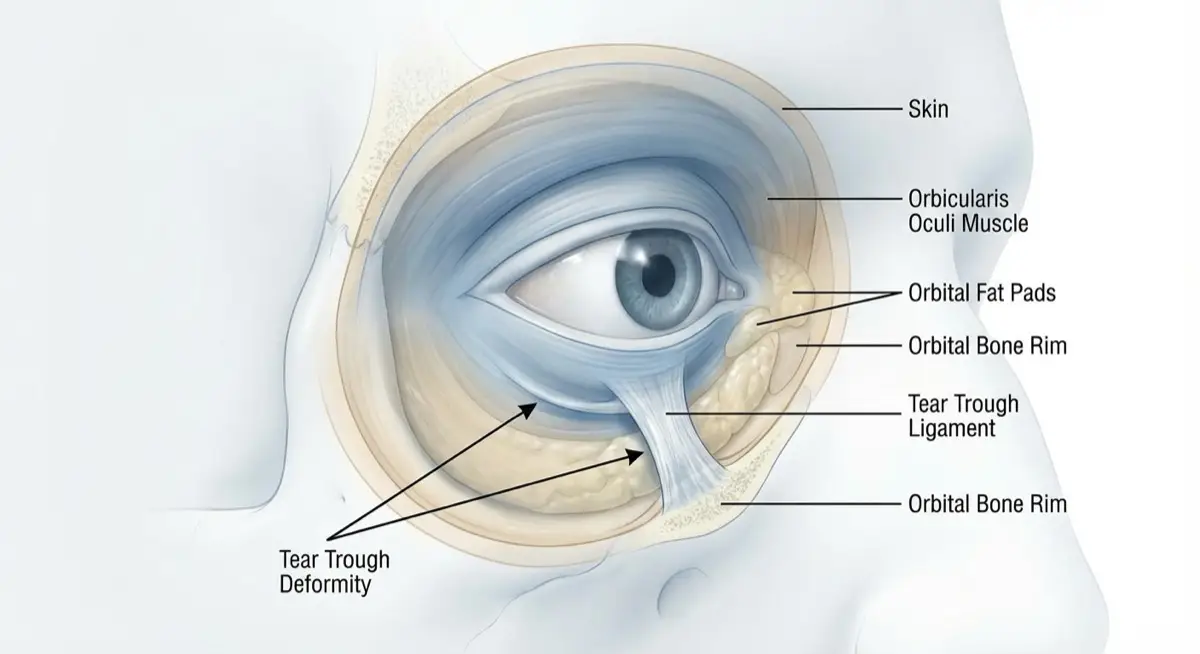
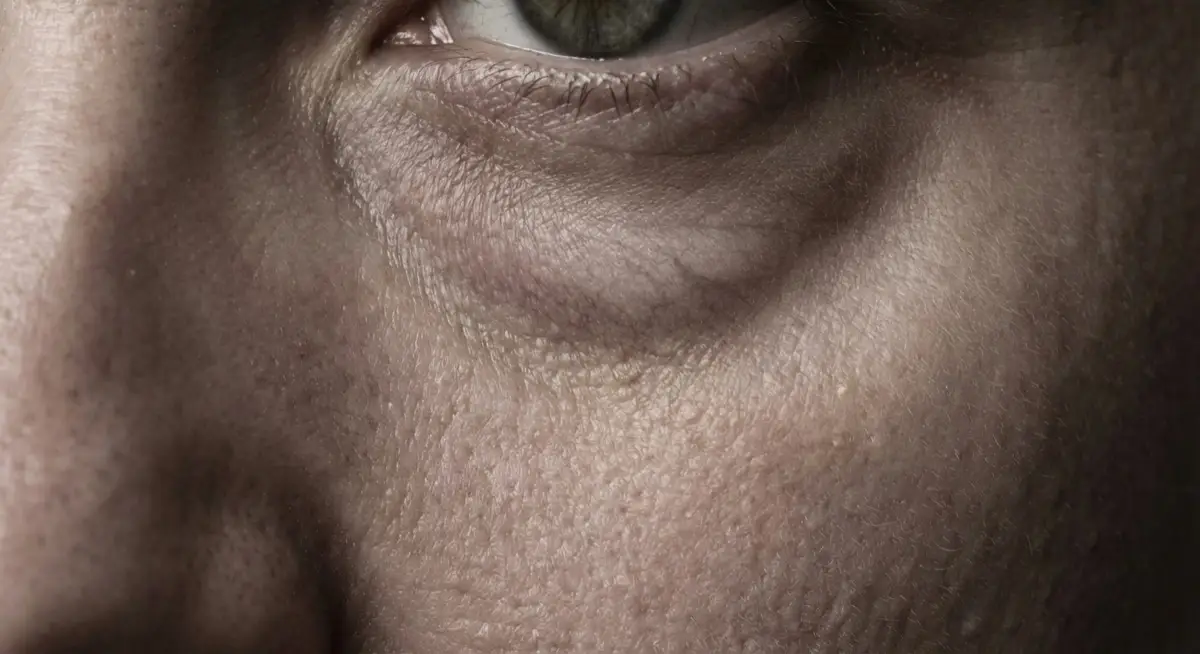
What Is Under-Eye Hollowing? Anatomy of the under-eye area: fat pads, muscle, bone, and the tear trough ligament Under-eye hollowing—clinically known as tear trough deformity—is the groove or depression that runs from the inner corner of the eye diagonally toward the cheek. While everyone has some degree of tear trough anatomy, it becomes a cosmetic concern when the groove deepens, creating shadows that make you look tired, aged, or unwell—even when you've had plenty of sleep. The tear trough is formed by a ligament that attaches the skin directly to the underlying bone.
Content Author & Reviewer
PRP London Clinic Medical Team
GMC-Registered Medical Professionals
Our team of GMC-registered medical professionals collaboratively review all medical content to ensure clinical accuracy and provide evidence-based information for patient education.




Last reviewed: February 8, 2026
What Is Under-Eye Hollowing?
What Causes Under-Eye Hollowing?
- Fat pad descent and atrophy — The orbital fat pads that cushion the eye socket shrink and drop with age
- Bone resorption — The orbital rim and maxilla (cheekbone) lose volume over time, reducing structural support
- Skin thinning — Loss of collagen makes the under-eye skin thinner, revealing underlying structures
- Genetics — Some people inherit prominent tear trough anatomy regardless of age
- Weight loss — Rapid or significant weight loss depletes facial fat, including the under-eye area
Can Under-Eye Hollowing Be Fixed?
The Foundation: Proper Assessment
- Grade of hollowing — Using the Barton Tear Trough Scale (Grade 1-4)
- Skin quality — Thickness, elasticity, and visible vascularity
- Fat pad position — Whether you have hollows, bags, or both
- Cheek support — Mid-face volume affects tear trough appearance
- Contraindications — Malar edema, festoons, or significant skin laxity may make injectables inappropriate
Our Treatment Approach
- Pathway 1: Regenerative — For mild hollowing or thin skin. Treatments like Polynucleotides, PRP, and Skin Boosters thicken the dermis and improve skin quality.
- Pathway 2: Volumising — For moderate hollowing requiring structural correction. EZ Gel Biofiller (100% natural) or HA Fillers (Teosyal, Juvederm) restore lost volume.
- Pathway 3: Surgical Referral — For severe hollowing with prominent fat pads (bags) or significant skin laxity. We provide honest referrals for lower lid blepharoplasty when surgery is the better option.
Who Experiences This Condition?
Common in
- •Individuals over 30 as natural ageing causes fat pad descent and bone resorption
- •Those with naturally thin skin in the periorbital area
- •People who have experienced significant or rapid weight loss
- •Individuals with genetic predisposition to prominent tear trough anatomy
- •Those with lower cheek volume (lack of mid-face support from below)
- •People with high cheekbones that accentuate the tear trough groove
Factors Affecting Severity
- •Depth of the natural orbital bone structure
- •Degree of subcutaneous fat loss in the mid-face
- •Skin thickness and elasticity in the periorbital area
- •Presence of adequate cheek (malar) support
- •Whether orbital fat pads have descended or herniated (forming bags)
- •Overall facial volume distribution and bone structure
Understanding Tear Trough Anatomy
To understand why under-eye hollowing occurs—and why certain treatments work—you need to understand the anatomy:
The Tear Trough Ligament This is a fibrous band that attaches the skin directly to the orbital rim (bone). It's the reason the tear trough groove exists—the skin is literally tethered down at this point.
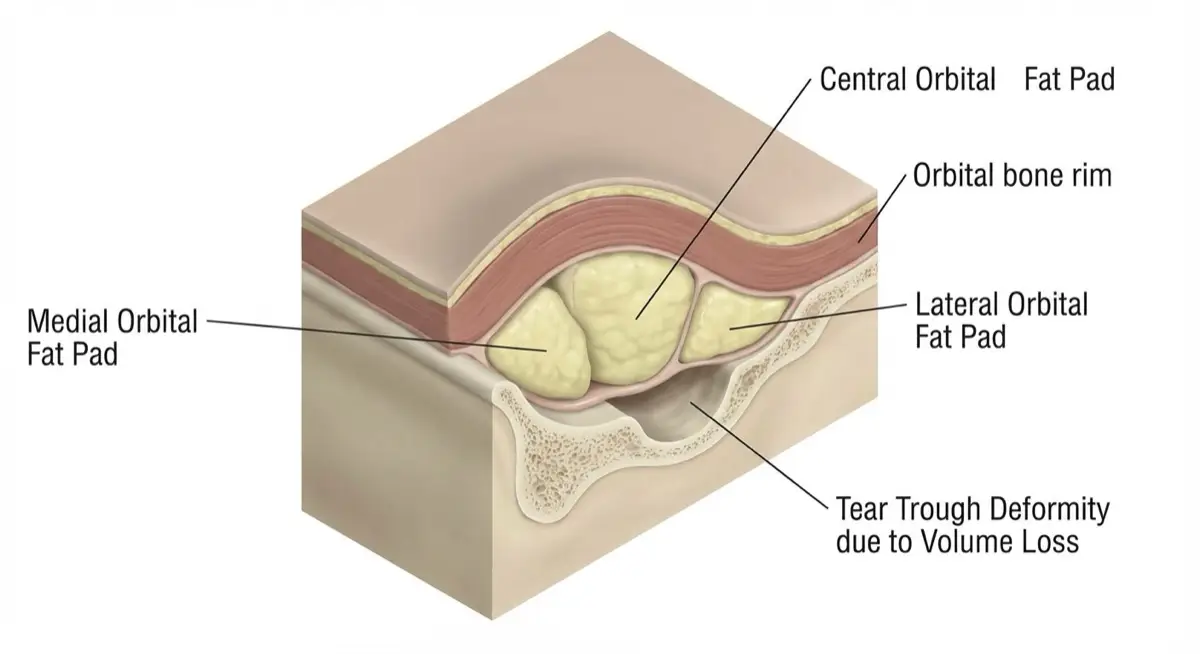
Orbital Fat Pads Three fat compartments sit above the tear trough ligament (in the lower eyelid). With age, these pads shrink and descend. When they herniate forward, they create 'bags.' When they simply shrink, they create hollowing.
SOOF (Sub-Orbicularis Oculi Fat) This deeper fat pad sits below the tear trough ligament, in the cheek area. When SOOF volume is lost, the tear trough deepens because there's less support from below.
The Orbital Rim The bone itself resorbs with age, particularly the maxilla (cheekbone) and orbital rim. This further reduces structural support, making hollows more prominent.
Why This Matters for Treatment Treatments work by either: (1) thickening the skin to hide underlying structures, (2) replacing lost fat pad volume, or (3) providing structural support where bone has resorbed. Your specific anatomy determines which approach—or combination—is right for you.
Ready to find your treatment path? Take our quick 3-question self-assessment.
Grades of Under-Eye Hollowing

Under-eye hollowing is clinically graded using the Barton Tear Trough Scale:
Grade 1 — Mild Subtle groove visible only in certain lighting. Minimal shadow. The transition from eyelid to cheek is slightly less smooth than ideal. Treatment approach: Regenerative (Polynucleotides, PRP, Skin Boosters)
Grade 2 — Moderate Clear groove visible in most lighting. Noticeable shadow creating a 'tired' appearance. The tear trough is obvious but skin quality remains reasonable. Treatment approach: Regenerative or mild volumising (EZ Gel, light HA filler)
Grade 3 — Significant Deep groove with prominent shadowing. Clear demarcation between lower eyelid and cheek. May have early signs of fat pad prominence (mild bags). Treatment approach: Volumising (EZ Gel or HA filler), possibly combined with regenerative treatments
Grade 4 — Severe Severe hollowing often combined with significant fat pad herniation (bags) and/or skin laxity. The combination of hollows AND bags creates a complex presentation. Treatment approach: Often requires surgical consultation (blepharoplasty). Injectables alone may worsen appearance in some cases.

During your consultation, we'll assess your specific grade and recommend the most appropriate treatment pathway.
Ready to find your treatment path? Take our quick 3-question self-assessment.
Why Eye Creams Won't Fix Under-Eye Hollowing
If you've tried every eye cream, serum, and home remedy but your under-eye hollowing refuses to improve, here's why:
Hollowing Is a Structural Problem
Under-eye hollowing is caused by volume loss—shrinking fat pads, bone resorption, and loss of structural support. No topical product can replace lost volume. It's like trying to fill a pothole by painting over it.
What Eye Creams CAN Do
- Temporarily plump the skin surface (hyaluronic acid)
- Reduce puffiness from fluid retention (caffeine)
- Improve skin texture over time (retinoids)
- Protect against further collagen loss (antioxidants, SPF)
What Eye Creams CANNOT Do
- Replace lost fat pad volume
- Lift descended tissue
- Fill the tear trough groove
- Reverse bone resorption
The Reality
Meaningful improvement in under-eye hollowing requires treatments that address the structural cause: either thickening the skin significantly (Polynucleotides, Sylfirm X), or physically replacing lost volume (fillers, EZ Gel). Skincare has a role—particularly retinoids for maintaining skin thickness and SPF for preventing further damage—but it's supportive, not corrective.
This isn't marketing—it's anatomy. Understanding this helps you invest your time and money in treatments that can actually make a difference.
Ready to find your treatment path? Take our quick 3-question self-assessment.
Under-Eye Hollowing Treatment Guide: Options by Severity
| Grade | Recommended Treatments | How It Works | Sessions |
|---|---|---|---|
| Grade 1 Mild groove | Polynucleotides Skin Boosters PRP | Thickens dermis, improves skin quality, subtle volumisation | 2-4 |
| Grade 2 Moderate hollow | EZ Gel Biofiller or light HA Filler | Replaces lost volume + stimulates collagen (EZ Gel) or immediate structural lift (HA) | 1-3 |
| Grade 3 Significant hollow | HA Filler (Teosyal, Juvederm) ± Polynucleotides | Structural correction with optional skin quality improvement | 1-2 |
| Grade 4 Severe + bags | Surgical Consultation (Blepharoplasty) | Removes/repositions fat pads, tightens skin—addresses what injectables cannot | N/A |
Important: This guide is for educational purposes. Treatment recommendations are made only after face-to-face assessment by a GMC-registered doctor, taking into account your anatomy, medical history, and goals.
Ready to find your treatment path? Take our quick 3-question self-assessment.
Filler vs Natural Alternatives: Which Is Right for You?
| Factor | EZ Gel Biofiller | HA Filler | Polynucleotides |
|---|---|---|---|
| Source | Your own blood (100% autologous) | Synthetic cross-linked HA | Purified salmon/trout DNA |
| Primary Effect | Volume + regeneration | Structural volume | Skin thickening |
| Best For | Mild-moderate hollowing, thin skin | Moderate-severe hollowing | Mild hollowing, skin quality |
| Longevity | 3-6 months | 9-12 months | 6-12 months (cumulative) |
| Tyndall Risk | None | Possible if superficial | None |
| Ideal Patient | Wants natural, no synthetics | Wants maximum correction | Wants skin improvement |
- Polynucleotides + PRP — Can thicken skin and provide subtle improvement, but won't fill deep structural hollows
- EZ Gel Biofiller — Technically a 'filler' but 100% your own material—no synthetic HA
- Sylfirm X — Builds collagen, thickens dermis—good for vascular shadows but won't replace volume
Our philosophy: We recommend what works for YOUR anatomy, not what's most popular or profitable. Many patients benefit from a combination approach.
Ready to find your treatment path? Take our quick 3-question self-assessment.
Why Are My Under-Eyes Blue After Filler? The Tyndall Effect Explained

If you've had under-eye filler and noticed a blue, grey, or purple tint that wasn't there before—you're likely experiencing the Tyndall Effect. This is one of the most common complications of tear trough filler, and understanding it can help you avoid it.
What Is the Tyndall Effect?
The Tyndall Effect occurs when hyaluronic acid (HA) filler is placed too superficially in thin skin. The filler particles scatter light, creating a bluish discolouration—similar to why the sky appears blue. In the under-eye area, where skin is extremely thin (just 0.5mm), this risk is heightened.
Why Does It Happen?
- Superficial placement — Filler placed too close to the skin surface rather than deep on the bone
- Wrong filler type — Using a dense, volumising filler instead of one designed for the delicate tear trough
- Overfilling — Too much product pushing upward toward the skin surface
- Thin skin — Patients with naturally thin periorbital skin are at higher risk
Can the Tyndall Effect Be Fixed?
Yes. The filler can be dissolved using hyaluronidase, an enzyme that breaks down HA. This is a straightforward in-clinic procedure. Once dissolved, the blue tint resolves and the area can be re-treated with proper technique if desired.
How We Avoid It
At PRP London Clinic, we prevent the Tyndall Effect through:
- Deep placement — Filler is placed on the bone (supraperiosteal), not superficially
- Appropriate products — We use fillers specifically engineered for the tear trough (Teosyal Redensity II, Juvederm Volbella)
- Cannula technique — Allows precise, deep placement with less trauma
- Conservative volumes — We under-fill rather than over-fill; you can always add more
- Alternative options — For very thin skin, we may recommend EZ Gel Biofiller or Polynucleotides which carry zero Tyndall risk
If you're experiencing the Tyndall Effect from treatment elsewhere, we can assess and advise on correction options.
Ready to find your treatment path? Take our quick 3-question self-assessment.
Malar Edema & Festoons: When Filler Isn't the Answer
Not everyone is a candidate for under-eye filler—and understanding why is crucial. Two conditions in particular can be made worse by injectable treatments: malar edema and festoons.
What Is Malar Edema?
Malar edema is chronic fluid accumulation in the cheek/under-eye area, causing persistent puffiness that's worse in the morning or after salty foods. It's different from fat pad herniation (bags)—it's fluid, not tissue.
Why filler makes it worse: Adding volume to an area with poor lymphatic drainage traps more fluid. Many patients have had filler elsewhere that triggered or worsened malar edema—and then seek more filler to 'fix' the problem, creating a vicious cycle.
What Are Festoons?
Festoons are hammock-like folds of lax skin and muscle that hang below the orbital rim, over the cheekbone. They're caused by weakened orbicularis oculi muscle and sun damage, not volume loss.
Why filler doesn't help: Festoons are a tissue laxity problem, not a volume problem. Filler cannot tighten loose skin—it can actually make festoons more prominent by pushing the lax tissue outward.
How We Screen for These Conditions
During your consultation, we specifically assess for:
- Fluid fluctuation (worse in morning vs evening)
- Response to gentle pressure (fluid displacement vs solid tissue)
- Skin laxity and muscle tone
- History of previous filler treatments
- History of allergies or sinus issues (associated with malar edema)
What We Recommend Instead
If you have malar edema or festoons, we'll be honest: filler isn't the answer. Depending on severity, we may recommend:
- Lymphatic drainage techniques and lifestyle modifications for mild malar edema
- RF treatments (Sylfirm X) for mild skin laxity
- Surgical consultation for significant festoons—we provide referrals to trusted oculoplastic surgeons
- Dissolving existing filler if previous treatments are contributing to the problem
Had a bad experience with filler elsewhere? We see many patients seeking correction. Honest assessment is the first step—book a consultation and we'll tell you what's actually going on.
Ready to find your treatment path? Take our quick 3-question self-assessment.
Why Choose PRP London Clinic for Under-Eye Treatment
The under-eye area is one of the most delicate and complex zones to treat. Here's why patients trust us:
Diagnostic-First Philosophy We don't sell treatments—we diagnose patients. Every consultation starts with anatomical assessment using the Tear Trough Grading Scale. We identify what's actually causing your concern before recommending any treatment.
Dual-Modality Expertise Our practitioners are trained in BOTH synthetic fillers AND regenerative medicine. This means we can offer the full spectrum of options—from HA fillers to EZ Gel to Polynucleotides—and recommend what's actually right for you.
GMC-Registered Medical Team All treatments are performed by GMC-registered doctors with specialist training in periorbital rejuvenation. The under-eye area is too complex for non-medical practitioners.
Safety-Focused Techniques We use micro-cannula techniques wherever appropriate to minimise bruising and protect the delicate vascular anatomy around the eye. Periorbital mapping ensures safe, natural-looking results.
Honest Referrals When surgery is the better option—for Grade 4 hollowing with significant bags or skin laxity—we'll tell you honestly and provide a referral to trusted oculoplastic surgeons. We won't recommend injectables when they're not appropriate.
Premium Products Only We use FDA-approved HA fillers (Teosyal Redensity II, Juvederm Volbella) and Class IIB medical devices (T-Lab PRF system). No compromises on quality.
Ready to find your treatment path? Take our quick 3-question self-assessment.
Treatment Process
Our under-eye hollowing treatment protocol follows a diagnostic-first approach:
Assessment: Grade & Cause Identification We use the Barton Tear Trough Scale and anatomical assessment to determine your specific grade and the underlying cause of hollowing.
Pathway 1: Regenerative (Mild Hollowing / Thin Skin) For Grade 1-2 hollowing or patients with thin, crepey skin: Polynucleotides, PRP therapy, Skin Boosters (Sunekos), Sylfirm X. These treatments thicken the dermis and improve skin quality.
Pathway 2: Volumising (Moderate-Severe Hollowing) For Grade 2-3 hollowing requiring structural correction:
- Natural preference: EZ Gel Biofiller (100% autologous, no synthetic materials)
- Maximum correction: HA Fillers (Teosyal Redensity II, Juvederm Volbella)
Pathway 3: Surgical Referral (Severe + Fat Pads) For Grade 4 hollowing with significant fat pad herniation or skin laxity, we provide honest referrals for lower lid blepharoplasty. Surgery addresses what injectables cannot.
Diagnosis & Assessment
Under-eye hollowing is assessed using the Barton Tear Trough Grading Scale (Grade 1-4) combined with anatomical examination. During consultation, we evaluate: the depth and extent of the tear trough groove, skin thickness and quality, presence of orbital fat pad herniation (bags), cheek volume and mid-face support, and suitability for different treatment approaches. We also screen for contraindications—malar edema, festoons, or significant skin laxity—that would make injectable treatments inappropriate. Understanding your specific grade and anatomy is essential for recommending the treatment that will actually work for you.
Prevention & Management
Lifestyle Tips
- •Maintain stable weight — rapid weight loss accelerates facial volume depletion
- •Protect skin from sun damage — UV exposure accelerates collagen breakdown and skin thinning
- •Stay hydrated — dehydration makes hollows appear more pronounced
- •Prioritise sleep — fatigue accentuates the tired appearance hollows create
- •Avoid smoking — accelerates skin ageing, collagen loss, and volume depletion
Home Care
- •Use colour-correcting concealer (peach/orange tones) to neutralise blue-grey shadows
- •Retinoids can help maintain skin thickness over time when used consistently
- •Caffeine-based eye creams may temporarily reduce puffiness but won't fill structural hollows
- •Good lighting and photography angles can minimise shadow appearance
- •Professional treatment is required for meaningful structural correction—no cream can replace lost volume
Not Sure Which Treatment is Right for You?
Our 3-question self-assessment helps guide you towards a suitable treatment option. Results are educational only—your consultation will confirm the best approach.
Verified Clinical Reputation
Ruby K
19 Jan 2026
Norin Hanifi
19 Jan 2026
Dominique Heslop
13 Jan 2026
lloyda221
06 Jan 2026
Mane Authority
06 Jan 2026
Victor Contreras Guerra
4 months ago
A A
5 months ago
harris jan
3 months ago
Independent Patient Feedback
Verify on Google Reviews →